Reablement is becoming an increasingly hot topic in the health and social care sector. As budgets continue to come under pressure, reablement offers a way to reduce costs for councils whilst maintaining peoples’ independence.
In 2018, we released an ebook that covered the basics of reablement. We have now produced this in a blog format so that you can easily find out the information you need on this topic. You can still download our PDF ebook for free, though, if you prefer.
What is reablement?
Sometimes, when people experience a sudden deterioration in their health or physical condition, they need help to adapt so that they are able to maintain independence and live full lives. This help, usually short and intensive, is called reablement.
Reablement is becoming increasingly important for people and for society overall. As health and social care costs increase, the focus for services is to encourage people to live independently in their own homes for as long as possible. Technically speaking, reablement is a form of ‘intermediate care’, which is a type of short-term support from health and social care services. Intermediate care as a whole is designed to encourage independence and prevent unnecessary hospital or care services admissions.
The remaining three types of intermediate care are:
- Crisis response – By definition, an assessment and short-term care that typically lasts 48 hours or less, and is designed to prevent a trip to hospital or a care facility.
- Home-based intermediate care – Services provided in a person’s own home or in their care home.
- Bed-based intermediate care – Services delivered in a hospital or care home.
Who can receive reablement?
Reablement is designed for people who have had a sudden change in their physical condition. They may have become disabled, suddenly frail from an illness, or they may be recovering from an accident. Reablement helps them perform normal, daily activities that we may take for granted, such as getting around the house, washing themselves or cooking. This may mean helping them adapt to their new physical condition and state of health, or relearning skills.Who exactly is eligible for reablement depends on the local authority.
Since one of the aims of reablement is to reduce costs to local services, resources tend to be targeted at people who are most likely to benefit physically from reablement. This means that individuals with severe mental illnesses, degenerative diseases, or who are receiving end of life care, are less likely to receive support. GPs or other health services can also refer people for reablement services.
Benefits of reablement
Many people benefit from reablement: the people using the service, their families, and their wider community.
The Social Care Institute for Excellence (SCIE) claims that reablement is typically welcomed by people receiving support, and they experience greater health and social care outcomes compared with those using home care. Their quality of life tends to be better, and their physical condition is more likely to improve.
Although we tend to talk of independence in terms of its benefit to local services, there is also the underestimated impact on the individual. Many people don’t like asking for help, and transitioning from being independent adults to being at least partly dependent on carers or family can be incredibly difficult.
Reablement allows these people to retain their pride and dignity. This means that their personal relationships are likely to be stronger. Although many families help members who are struggling physically, it can sometimes place strain on their relationships. Maintaining a person’s independence helps them, in turn, maintain strong relationship with their family, their friends and their local community. This prevents social isolation and loneliness.
The reablement process
- Assessment: Reablement starts with an assessment, usually by a healthcare professional, of whether a person may benefit from it. The assessment will take into account factors such as the person’s mobility, what skills they still have, their physical strength, and their ability to perform basic tasks such as cooking and washing.
- Frequent, longer visits: The purpose of reablement is to help a person very quickly become independent once again. This means that reablement workers may make frequent visits, but it also means they are less likely to intervene in the performance of tasks than a traditional care worker. They are more likely to observe and encourage, only taking over or helping directly when necessary. These visits are therefore likely to be longer than normal care visits. Workers may be specifically trained in reablement, but they may also be physiotherapists or occupational therapists.
- More assessments: Reablement workers aim to help a person regain their independence as quickly as possible. They will assess often to determine when the person no longer needs support.
- Adjustments or Equipment: The reablement workers, or an occupational therapist, may recommend that adjustments be made to a person’s home or that assistive aids be introduced to help them remain independent. Such aids may include a stairlift or support bars in the bathroom.
- Forward Planning: If done properly, the planning for what happens after reablement ends should begin at the very start of the process. This planning will involve healthcare professionals, the reablement workers, the individual receiving support, and any family or friends who may be involved in any ongoing care and treatment.
The impact of reablement

Reablement has been an active policy since 2010. SCIE have reviewed the impact of reablement across numerous independent and official studies and have found that it has had an overall positive effect. They concluded:
- Reablement is becoming a ‘default’ service whenever needs are identified, rather than just being available to those leaving hospital.
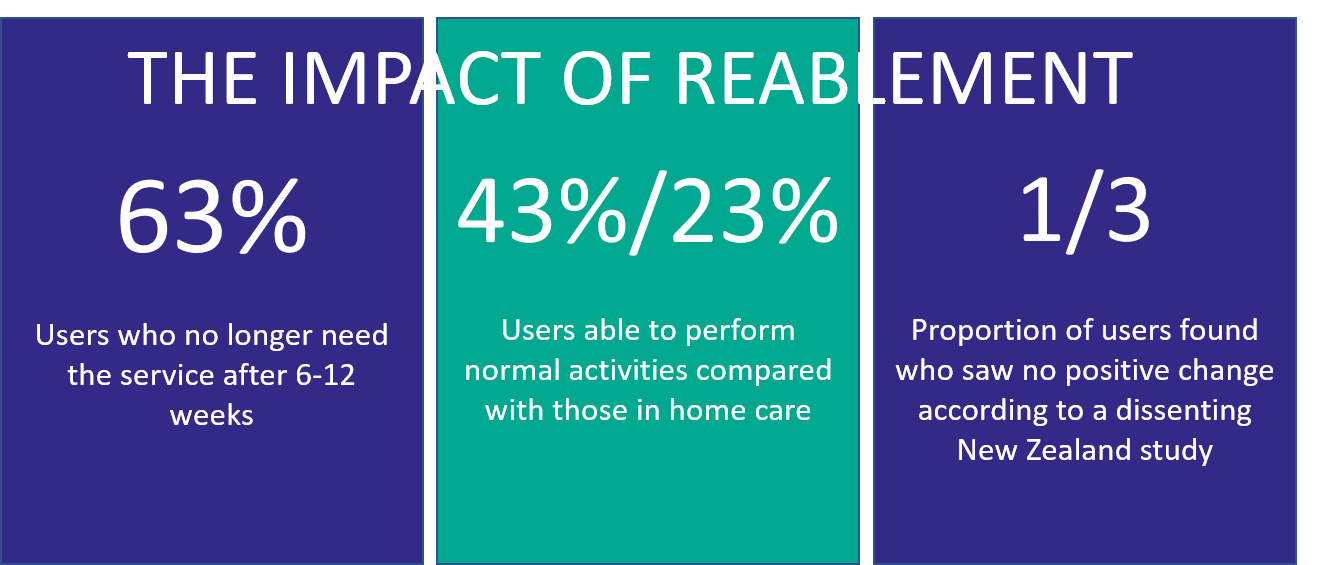
- 63% of reablement users no longer need the service after 6-12 weeks.
- People and families appear to have welcomed reablement. People in the study seemed to have been particularly pleased with the speed of the service.
- Reablement is proving likely to be cost-effective by reducing long-term care costs. Although the upfront costs are higher (on average £2000 for reablement compared to £1,392 for 6 weeks of home care), 26% of users had a reduced need for home care hours after going through the process. The overall need for care services is reduced by 60%.
Nevertheless, some issues were noted. Some people felt that they were not given enough assistance with performing domestic tasks at the start of the reablement process. There was also a concern that some of the reablement ‘ethos’ was lost in handovers between service providers.
SCIE have also noted that the skills required for reablement are very different from those required for traditional care work. For example, reablement staff are required to observe and watch rather than directly intervene, a skill that can be difficult for someone used to helping others. There is also a need for “active reassessment” at every session to track progress and identify need. Reablement workers also require more flexible working practices than is typical, since it’s important that the reablement worker(s) visiting the individual remains consistent. Managers and supervisors need to ensure any staff participating in reablement work have the appropriate training.
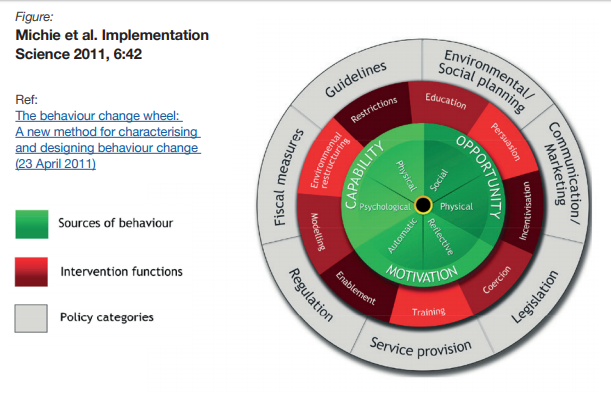
Perhaps the most interesting point from SCIE’s research summary, though, is that individuals receiving support need to change their expectations and attitudes if reablement is to work properly: “reablement was considered to be more successful if service users were motivated – ‘people have got to want to do it.” The reablement worker could be crucial here as a motivator, and managers and supervisors may wish to ensure reablement workers have positive outlooks themselves.
The remaining questions
Reablement is a relatively new concept in social care and there are still some questions that require more research. The National Institute for Health and Care Excellence (NICE) released a paper in 2017 outlining some of these questions:
- How effective is reablement for people with dementia? Although local authorities are currently less likely to provide reablement services to people with dementia, there is still little evidence or research as to whether those with early stage dementia – or their families or carers – may benefit.
- How effective and cost effective are repeated periods of reablement, and reablement that lasts longer than 6 weeks? Although this document has assumed a single period of reablement, there is no technical limit to how often reablement services may be provided to a person. In practice, reablement is only funded for 6 weeks, even if sometimes it is offered for longer and more frequently. Therefore, there are no studies as to whether these extended periods of support are cost effective or deliver better outcomes for the individual.
Further resources








 The Government published its long-term plan for the NHS this week. We’ve looked at what it means for mandatory, clinical and specialist training for the next decade:
The Government published its long-term plan for the NHS this week. We’ve looked at what it means for mandatory, clinical and specialist training for the next decade: