Person-centred care should be at the heart of any health and social care provider’s approach to care. But how do we embed it into training and development? The person-centred approach framework released by Skills for Health, Skills for Care and Health Education England includes a section advising organisations on how to embed these approaches using training and development. The framework recommends a number of “underpinning principles” to guide an organisation’s approach to training and development on the topic.
Behaviour change
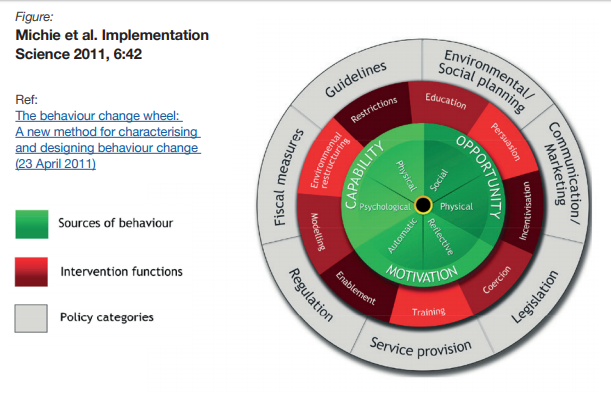
The most important of those principles is “behaviour change”. As with the whole idea of a person-centred approach, this concept is now fairly old, but its implications have still not been felt by a vast number of organisations in the sector, and indeed across all sectors. Unfortunately, the framework is frustratingly light on how behaviour can be changed in a positive way, reflecting only that it is more successful than “isolated training”. It does note, however, that any training geared towards changing behaviour will fail if the organisation’s structure and processes reward an old, habitual behaviours rather than reward the behaviours enshrined in the framework:
Development of capability must simultaneously be supported with the right processes, system and opportunity together with locally relevant incentives, which build those intrinsic and extrinsic motivations.
Co-producing training
The framework also recommends that training is co-produced to a certain extent. This boils down to having the carer or even the service user contributing stories and reflections about their experiences during the course, or even during the planning of the course.
This shouldn’t be new to any good provider or trainer. A good trainer will seek to engage the people on the course, getting them to talk about how they can relate to content of the course and whether they can think back to any relevant experiences. A classic reflection exercise is ‘What would you have done differently?’, getting the learner to retrospectively apply their new learnings to a previous experience.
Again, the framework highlights that the best co-produced training will have people involved in the planning stage without them even knowing it, with HR processes that continuously seek feedback from service users and staff.
Reflective practice
Again, we are all familiar with the importance of getting members of the team to reflect on what is working, what isn’t working, and on the needs of others.
The challenge for many health and social care providers, of course, will be finding the time for members of staff (including managers) to engage in reflective practice. As resources become more stretched, it will become more and more difficult. One possible solution is to stress its importance during the induction period, to effectively train staff to continuously reflect ‘on the job’.
Continuous improvement
The framework focuses on the structural element of continuous improvement – of managers consistently providing feedback to staff. The framework does not mention, though, the significance of a continuous improvement culture. The best companies in industry that practice continuous improvement have it as part of their culture, running through everything they do, encompassing HR, finance, production and service delivery processes.
Achieving culture change, of course, is difficult to accomplish and can take a long period of time. It requires concentrated effort and the full support of senior leadership. As any continuous improvement organisation will tell you though – and this includes the likes of General Electric and Mitsubishi – it is well worth it.
Value-based approaches
This part of the framework primarily refers to recruitment and retention. Unfortunately, the section of the framework seems a little too aspirational. The news this week has been full of reports about the huge number of vacancies with the NHS, with retention proving as much of an issue as recruitment. This is compounded by applications from the EU dropping off significantly in anticipation of Brexit and the end of free movement. Even a brief perusal of any job site will tell you that care settings are also continuously recruiting in a sector renowned for its high staff turnover.
Increasingly, health and social care providers are taking what they can get. Recruiting on the grounds of values and outlook, as the framework advocates, is simply not possible for those who cannot afford to go and do it. The emphasis has to be on training and induction. This is helped by having a strong culture that new workers can be embedded in to quickly.
Methods for delivering training
The ‘narrative’ section of the framework does not elaborate on this principle much, although content further down in the document does by discussing “permitted time for e-learning”. As ever, the key is deciding which approach is most suited for each person and for each subject area. E-learning is often perfect for entry-level staff being trained in compliance topics where answers are often binary (i.e. yes or no, right or wrong). It may not be suitable for training that requires reflection and where judgement may be more subjective.
Conclusion
Although the framework raises some great points, it does feel a little too aspirational and abstract at times. Many health and social care providers will feel that it doesn’t account for challenges in recruitment and funding issues. If you take anything from the framework and this post, let it be these three points:
- Culture, culture, culture: if behavioural change, continuous improvement and a person-centred approach are going to take hold, it needs to be embedded in your culture.
- The method of training delivery needs to be suitable for the person and the subject area.
- Train people to reflect on their work every day and ‘on the job’. This embeds it into their behaviour, and means they are doing it even if you can’t set aside specific time for them to do so.