European Union General Data Protection Regulations
The EU GDPR is designed to help all of us have more control over our personal data, and how is it used.
Who does the information GDPR apply to?
Data subjects, being all visitors and users of any website who are members of the European Union, and therefore who submit personal data. advantageaccreditation.com is the data processor and data controller of this site. You can find out more about this law here.
Privacy Policy
Effective from 25th May, 2018
This Privacy Policy sets out how we use and protect information that you may provide when you use this website. Your privacy is protected and important to us. If you provide identifiable personal information it will only be used to help us respond to your requests and to help you get the most from our services.
advantageaccreditation.com collects any personal data submitted through https://advantageaccreditation.com
We may update this policy periodically, please check this page to ensure that you are in agreement with any changes.
What we Collect
Personal information, basically any data that can be used to identify or contact you is collected so we can respond to your needs. This could include your name, business name, address details, email, telephone numbers, or information pertaining to your enquiries. You may also at times be asked to leave a message about your enquiry. Websites also collect your IP address through the use of Cookies (find out more about cookies below).
If you opted-in to our mailing list, you may receive occasional emails on important updates or service information. You have the right to opt-out or and have any personal details removed at any time, please email [email protected]
What We Do With The Information We Collect
Information is saved until the enquiry is dealt with, and then archived with the project or on cloud based systems if you are an involved in ongoing projects. We also retain your contact details and information in the emails you have sent, but you can request to have your personal details deleted at any time.
We will not sell, distribute, or lease your personal information to third parties unless we have your express permission, or are required by law to do so. We may use your personal information to send you relevant information about our services.
Data Security
In our commitment to ensuring that your information is secure and to prevent unauthorised access or disclosure, we have suitable physical, electronic and managerial procedures in place to safeguard and secure the information we collect online.
- Data is stored on a secure cloud-based server or on a secure, password protected computer with limited user access.
- Sending information over the internet is generally not completely secure, and we can’t guarantee the security of your data while it’s in transit. Any data you send is at your own risk.
- We have procedures including passwords, restricted access and other security features in place to keep your data secure once we receive it.
- advantageaccreditation.com will NEVER pass on your personal data to third parties without first getting your explicit consent.
Controlling your personal information
You may choose to restrict the collection or use of your personal information in the following ways:
- Whenever you are asked to fill in a form on the website, look for the box that you can click to indicate that you do not want the information to be used for direct marketing purposes
- If you have previously opted-in to a mailing list, or provided other information, you can find out what information we hold, and ask us to remove or not to use any of it, by writing to, or emailing [email protected]
- You may request details of personal information which we hold about you.
- If you believe that any information we are holding on you is incorrect or incomplete, please write to, or email us as soon as possible: [email protected] we will promptly correct any information.
Google Analytics
User and Event Data Retention
User-level and event-level data associated with Google Analytics cookies is retained for 14 months and then automatically deleted.
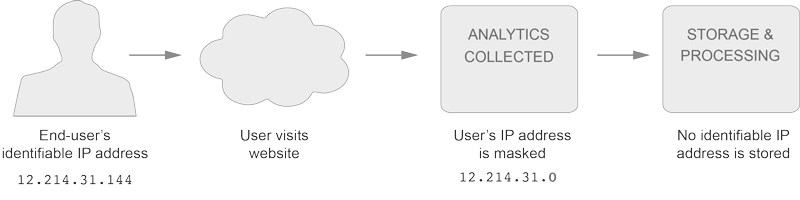
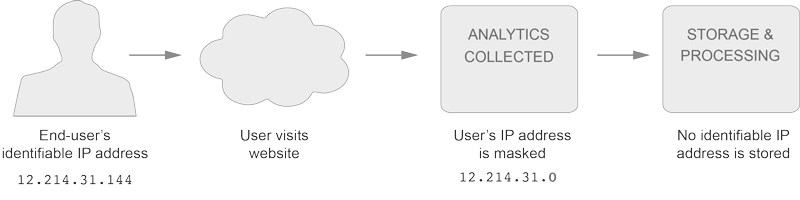
IP Anonymization
We have implemented IP Anonymization, simply put, the last three digits of your IP address are set to zeros in memory shortly after being sent to the Analytics Collection Network. The full IP address is never written retained, or written to disk.
Cookies
This site also uses cookies to improve your user experience, find out more or manage them here.