Although the media will no doubt focus on the negatives, a new CQC report on the state of care in mental health services has actually uncovered a lot of good news. A study of mental health services conducted between 2014 and 2017 has found that 68% of core services provided by the NHS are...
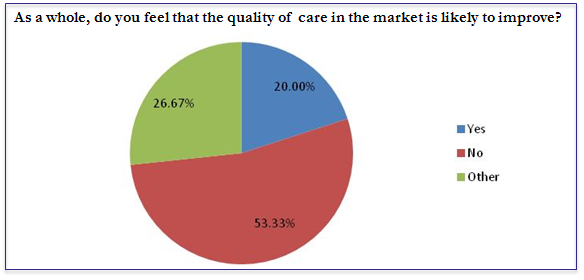
Many pessimistic about the future of care
The results of an Advantage survey for a new report on the Future of Care show that many in the care sector are pessimistic about the future of the sector and the quality of care. The survey asked respondents to rate their optimism about the future of the sector out of 10, with 10 being...
Did you know about Skills for Care’s Leadership Programme?
Skills for Care are ramping up the publicity on their Leadership Programme, which is open to applications. Skills for Care have a raft of leadership programmes (with a discount for members) that many seem unaware of. Although it can be hard to take time out of an organisation, it’s always important to ‘sharpen the...
SCIE makes the case for intermediate care
The Social Institute for Excellence has published a new highlights paper on how intermediate care can deliver better outcomes for people in care. The report has found that effective intermediate care reduces pressure on hospitals and on social care settings. For example, it has found that 72% of people who received intermediate care did...
Person-centred approach – training and development
Person-centred care should be at the heart of any health and social care provider’s approach to care. But how do we embed it into training and development? The person-centred approach framework released by Skills for Health, Skills for Care and Health Education England includes a section advising organisations on how to embed these approaches using...
Person-centred approaches in healthcare
A new framework is being launched by Skills for Health, Skills for Care and Health Education England to put people-centred approaches at the heart of the health and social care sector. The framework builds on a long-running trend to put people and their needs at the heart of health and social care, replacing the...
Choosing the perfect care home
BBC News have published an article online today advising people on ‘how to choose the perfect care home‘. We liked the article because it included a checklist from Age UK on what to ask potential residential or nursing homes before you or your family member moves in. The list is useful for providers though,...
Is DoLS set to be replaced?
This may have slipped under everyone’s radar. A report that received little attention in the news from the Law Commission has recommended scrapping the current Deprivation of Liberties Safeguards, which it describes as “in crisis”, and replacing them with a new Liberty Protection Safeguards system. Although this may seem like semantics, the new system...
New report shows the importance of basic skills
A number of news outlets are leading today with the news that the CQC has found that 32% of nursing homes in England and Wales are failing on safety:Inspectors making unannounced visits to care homes found medicines being administered unsafely, alarm calls going unanswered and residents not getting help to eat or use the...
The biggest problem with training, and what you can do about it
We've all been on a training course of some form or another. It might be something compliance based - like health and safety - or something that really impacts on how we perform in our role. The problem, however, is that it often isn't built around the learner. The reason why is clear: training...
The best health and social care resources
Finding up to date information on health and social care can be hard. If you're in a position where you're responsible for providing training into the sector, it can be time consuming trying to keep track of regulation and best practice changes, as well as keeping your own CPD going.So, to give you a...
No stop for health and social care integration efforts
The head of NHS England has signalled that there is no intention of ending plans to more closely link the British health and social care systems. A report from the National Audit Office earlier this year suggested that health and social care integration was not being carried out effectively enough to deliver the desired...
A look at Teeside’s ‘outstanding’ care home
Nunthorpe Care Home in Middlesbrough has just received the highest rating possible from the CQC of ‘outstanding’. How did it do it? According to its residents and the CQC report, a “homely” feel, stimulating activities, and a passionate workforce. Take a closer look by clicking here …...
New start-up presents new model for care
A new start-up is seeking to let more people with dementia live in their own home by using technology. Adam and Daniel Pike started SuperCarers in response to their own family’s experience with dementia. Their grandmother suffered with the disease, but preferred to stay in her own home. Lacking the finances to pay for...
Care crisis: funding alone not the solution
A piece in The Guardian has highlighted that funding alone will not be the solution to the country’s care crisis. Instead, focusing on talent within the sector will be the key. The article by Paul Dosset calls for a radical rethink of “our strategy towards the health and happiness of the British people”. A...