New CQC Quality Statements
The Care Quality Commission (CQC) have introduced a new strategy for assessing health and social care providers. The new assessment framework can be used to investigate care providers, local authorities and integrated care systems.
The CQC’s new quality statements establish clear goals for care providers to ensure high-quality, person-centred care across the sector. These statements replace the Key Lines of Enquiry (KLOEs). Each statement relates to specific CQC regulations. The new quality statements are:
Safe

Learning culture
Care providers, local authorities and integrated care systems should ensure service users and staff are listened to when raising safety concerns. Any safety events should be investigated and reported with the goal of learning from mistakes and adapting care delivery to prevent further risks.
Safe systems, pathways and transitions
Any transitions, e.g. from one service to another, should be monitored and managed carefully.
Safeguarding
Staff must protect service users’ rights to safety, free from harm, harassment, abuse, neglect and discrimination. They should enable all people to share any concerns.
Involving people to manage risks
Providers should meet needs safely, allowing service users to have as much choice as possible according to legislation.
Safe environments
The care environment, including equipment, facilities and technology, should promote safety and not risk harm.
Safe and effective staffing
There should be enough members of staff who have appropriate skills, qualifications and experience. Staff should work together well and receive the right supervision and opportunities for development.
Infection prevention and control
All staff should be able to manage risk of infection and share any concerns with appropriate agencies.
Medicines optimisation
Any medication should be kept safe and used appropriately to meet needs.
Effective

Assessing needs
Needs of service users should be continually assessed and reviewed. Staff should consider the individual’s own wishes too.
Delivering evidence-based care and treatment
All care should be delivered in-line with relevant legislation and evidence-based good practice and standards.
How staff, teams and services work together
Staff should work together well to create and effective service. Information about service users can be shared between services.
Supporting people to live healthier lives
People should have every opportunity to maximise their independence.
Monitoring and improving outcomes
Providers should continually check outcomes are positive, consistent and meet expectations.
Consent to care and treatment
All service users must understand their right to consent where possible, and all staff should respect their decisions.
Caring

Kindness, compassion and dignity
All staff should show kindness, empathy and respect to service users and colleagues.
Treating people as individuals
Providers should meet individuals’ needs and preferences while considering their unique strengths, aspirations, and culture.
Independence, choice and control
Service users should be aware of their rights and be given a choice about their care and treatment.
Responding to people’s immediate needs
Staff should listen to individuals’ needs and wishes and respond in the moment to minimise discomfort or distress.
Workforce wellbeing and enablement
Providers should promote wellbeing for all staff.
Responsive

Person-centred care
The individual must be at the centre of care and treatment choices. Staff should involve service users in care decisions and respond to their unique needs.
Care provision, integration, and continuity
All care and treatment should be flexible to support choice and meet diverse needs.
Providing information
Staff should provide accurate, understandable information to people in their care.
Listening to and involving people
Providers should create opportunities for service users to raise complaints and present ideas.
Equity in access
All people should be able to access the care they need when they need it.
Equity in experiences and outcomes
Providers should listen to service users most likely to experience inequality and respond to their needs and concerns.
Planning for the future
Service users should make plans for their own life, including end of life care.
Well-led

Shared direction and culture
Leaders should consider equality, rights, and challenges in their organisation community.
Capable, compassionate and inclusive leaders
In all levels of leadership, staff should have the right qualities including skills, knowledge, credibility, integrity and openness.
Freedom to speak up
Leaders should ensure all people feel heard when raising comments and concerns.
Workforce equality, diversity and inclusion
Staff should be able to work in an inclusive and fair culture.
Governance, management and sustainability
Leaders should provide staff with clear roles and responsibilities. They should act on information about risk and outcomes appropriately.
Partnerships and communities
Staff have a duty to collaborate, sharing information between services.
Learning, improvement and innovation
Leaders should strive for continuous improvement and contribute to research and development.
Evidence Categories
Alongside the new quality statements, the CQC have introduced a new set of evidence categories. Not all of these will be used in all assessments. The categories used will depend on the service type, level of assessment and whether the assessment is for an existing service or registration. The six evidence categories are:
People's experience of health and care services
The CQC considers the experiences of people using the service, or their family, friends or advocates. Anything negative is reviewed further. The sources considered while factoring in demographics, inequalities and frequency of use of care services.
Feedback from staff and leaders
Information is collected from staff using surveys, interviews, focus groups and compliments or complaints raised previously.
Feedback from partners
Information is collected from organisations that interact with the service being assessed, such as commissioners, local providers, professional regulators, accreditation bodies and multi-agency bodies.
Observation
This can be on-site, off-site or both. On-site inspections include observing care, speaking to people, and reviewing the environment. Off-site observations may involve interviews and calls with staff, service users and the community.
Processes
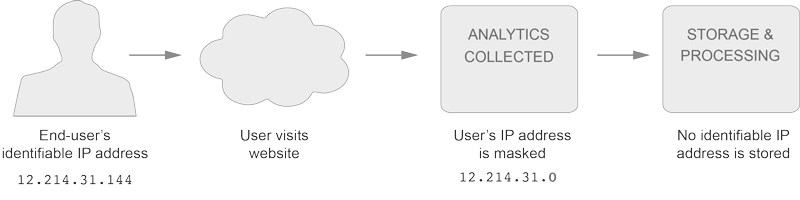
The CQC check how effective policies and procedures are, considering data from national clinical audits, patient level data sets, waiting times, infection prevention and control, reported incidents and care records.
Outcomes
These include mortality rates, readmission rates, emergency admission rates, patient reported outcome measures, infection control rates, and quality of life assessments.
As an accreditation body specialising in health and social care, we are careful to stay up-to-date with news within the sector. You can read more helpful guidance here.